Abnormal Uterine Bleeding - ppt video online download
$ 17.50 · 4.7 (360) · In stock
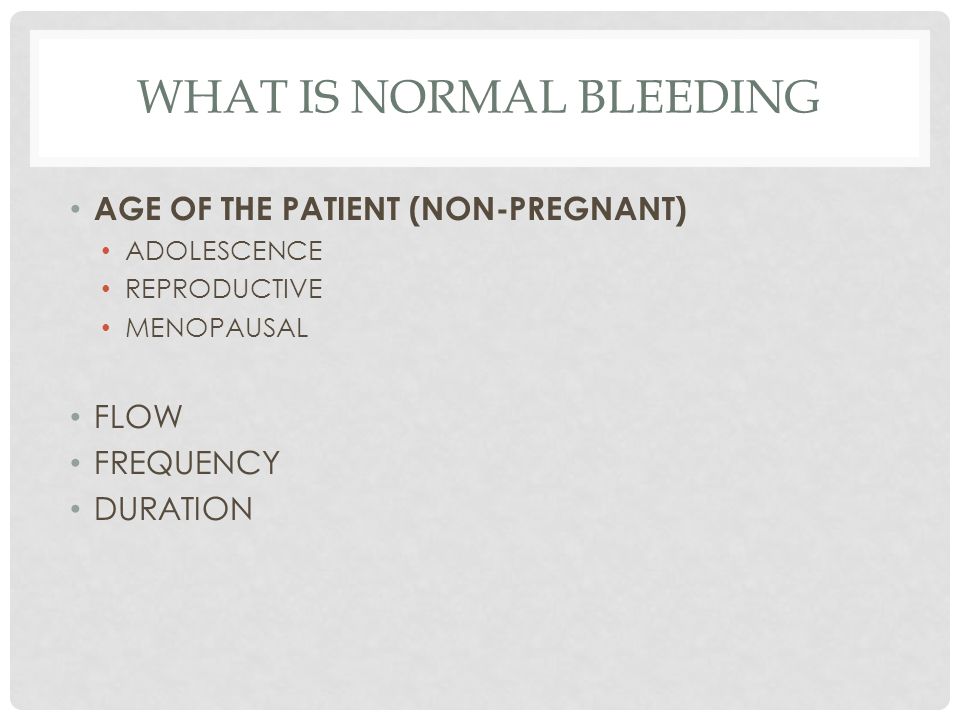
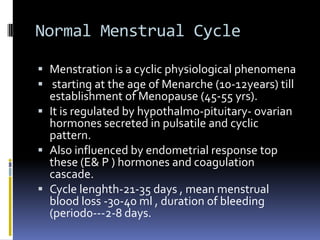
Abnormal Uterine Bleeding Definitions: Normal menstruation is defined as occurring every days, lasting 3-7 days and resulting in an average mbl (menstrual blood loss) of 35 ml. Menorrhagia is defined subjectively as excessive, prolonged and regular MBL and defined objectively as MBLof 80 ml or more. Metrorrhagia is defined as regular IMB. Menometrorrhagia is defined as prolonged menses and IMB Polymenorrhoea is defined as menses occurring of < 21 days. Oligomenorrhoea is defined as menses occurring of > 35 days. Amenorrhea is defined as absence of menstruation for > 6 months.
Definitions: Normal menstruation is defined as occurring every days, lasting 3-7 days and resulting in an average mbl (menstrual blood loss) of 35 ml. Menorrhagia is defined subjectively as excessive, prolonged and regular MBL and defined objectively as MBLof 80 ml or more. Metrorrhagia is defined as regular IMB. Menometrorrhagia is defined as prolonged menses and IMB. Polymenorrhoea is defined as menses occurring of < 21 days. Oligomenorrhoea is defined as menses occurring of > 35 days. Amenorrhea is defined as absence of menstruation for > 6 months.
Menorrhagia is one of the commonest causes of referral to gynecological clinics, is the commonest indication for hysterectomy, and the commonest cause for fe-deficiency anaemia in developed countries. Aetiology: Dysfunctional uterine bleeding i.e DUB (non-organic menorrhagia): 60% of cases. Is defined as excessive MBL in the absence of organic,(genital & systemic) diseases. Ovulatory DUB: 85 % of cases. Occurs at reproductive age. The cause is a disorder in the endometrial function i.e endometrial prostaglandin imbalance (↑ PGE2/ ↓PGF2α ratio) & increased endometrial fibrinolytic activity. Anovulatory DUB: 15% of cases. Mostly occurs at extremes of reproductive age. In the reproductive age occurs in chronic anovulation as in PCOS.
Is defined as excessive MBL due to organic causes i.e genital or systemic. Genital causes: 35 % of cases. Uterine: Fibroids (submucous type), endometrial hyperplasia & carcinoma. Adenomyosis & endometriosis. PID. Cu-releasing IUCD. Theca & granulose cell tumours of ovary. Systemic causes: <5% of cases. Thyroid Drugs: Anticoagulants, aspirin ,tamoxifen. disorders : Myxaedema. Blood disorders: ITP, deficiency of coagulation factors, Von-Willebrand s disease and Glanzman disease. Liver failure.
In clinical practice ,diagnosis depends on the subjective complaint. Objective measurements of the MBL using alkaline-haematin method is not used in clinical practice. So a comprehensive history is vital in order to minimize the false positive rate of the subjective diagnosis. NB. If the MBL was assessed objectively using alkaline-haematin method, it is found that 40% of patients who were diagnosed subjectively to have menorrhagia DO NOT, and 20% who were diagnosed to have normal menses have menorrhagia. Analysis of the complaint and associated symptoms: Duration of the complaint. Regularity of the cycles. Days of the menses , Passage of the clots , Number and size of sanitary pads. Restriction of activity. Associated : IMB , PCB. Associated : congestive dysmenorrhea, pelvic pain , vaginal discharge and dysparunnia.
Previous investigations and treatment for her complaint: Previous investigations : CBC, U/S, TFT and endometrial biopsy. Previous treatment : Drugs , Mirena. Gynaecological history: Contraception: Hormonal , Cu-releasing device. Last cervical smear . Previous gynecological operations. Medical history: Drugs: Anticoagulants , Aspirin , Tamoxifen. Thyroid disorders: Myxaedema. Blood disorders: ITP, deficiency of coagulation factors, Von-Willebrand s disease and Glanzman disease.
General: signs of anemia, weight, hair distribution, thyroid , breast examination and pelviabdominal masses. Pelvic: Speculum examination of the cervix & vagina. Bimanual examination of the uterine size & shape , and adnexal masses. Investigations: Initial investigations. U/S. CBC. TFT. Endometrial biopsy : Mandatory in above 40 years patients to exclude endometrial Cancer. Best : by hysteroscopy directed endometrial biopsy. Others: D&C or out-patient aspiration endometrial biopsy. Rarely –coagulation screening in suspicion of blood diseases.
Treatment depends on the age, underlying cause, & desire to maintain fertility. Treatment of acute menorrhagia: Treatment of aneamia. Hormonal. Best by –oral progestogen in high dose e.g norethisterone 10 mg /t.d.s. Others : GnRH analogues, Danazol and Primarine I.V. D&C in cases not responding to hormonal treatment. Treatment of chronic menorrhagia. Organic menorrhagia: Treatment depends on the underlying cause.
Treatment of anemia. Drugs. Non-hormonal: Anti PG, Antifibrinolytic. Hormonal: Hormones in use : Oral progestogen, COC. Hormones not in use: GnRH analogues, Danazol Childbearing age menorrhgia: Drugs – as above. Mirena: (Progestogen releasing IUCD)
Treatment of anemia. Drugs – as above. Mirena: (Progestogen releasing IUCD. Surgical treatment. Hysterectomy . Endometrial resection and ablation.
Efficacy: Reduce MBL by 25 % Dose: 500 mg/t.d.s for 5 days during days of menses. Side effects: Gastritis & gastric bleeding, therefore should not be given to patients with H/O gastritis and peptic ulcer. Antifibrinolytic agents- e.g Tranexamic acid. Efficacy: Reduce MBL by 50% Dose: 0.5 – 1 gm / t.d.s for 5 days during days of menses. Side effects: Nausea & vomiting , and rarely intracranial thrombosis & central venous stasis retinopathy, therefore it is contraindicated in H/O thromboembolism. Combined oral contraception. Reduce MBL by 50 %
Given in a dose of 5 mg twice daily, from day 5 to day 25 of the cycle. Are less effective in ovulatory menorrhagia , and when used in ovulatory menorrhagia , it should be given in larger doses i.e 5 mg/t.d.s. Side effects: - Bloating and increase weight. - Headache. - Nausea and vomiting. - Osteoprosis in long term treatment. - Others: acne, hirsutism, breast tenderness & decrease libido. NB: Oral progestogens, is the most safe and most common used hormonal treatment in all ages, due to absence of serious side effects.
Is a synthetic androgen derived from 19-nortestosterone with antioestrogenic, antiprogestogenic & androgenic activities. Action is similar to danazol, and the efficacy and side effects are also similar to danazol, so it is NOT used in the treatment of menorrhagia . Dose : 2.5 mg / twice weekly. Mirena (Progestogen releasing IUCD ) Action : Release 20 μg daily of levonorgestrol which induces endometrial atrophy. Efficacy : Marked reduction of MBL by %, so that it can be considered as a valuable alternative to drug treatment and surgery. Other advantages: Very effective contraception – most effective reversible contraceptive method. Reduce the incidence of PID. Does not increase the risk of ectopic pregnancy. Side effects: Breakthrough bleeding & spotting in the first few months after insertion.
It involves endometrial resection & ablation to induce a fibrous tissue layer i.e iatrogenic Asherman s syndrome. The methods used include : diathermy, laser, radiofrequency induced ablation & thermal balloon ablation. Efficacy: Amenorrhoea in 50 %, marked reduction in MBL in 30%, & no improvement in 20% of patients. Advantages compared to hysterectomy: Shorter stay in hospital i.e day case operation compared to 3-7 days stay in hysterectomy. Shorter return to normal activities i.e 1-2 weeks compared to 6-8 weeks in hysterectomy. Fewer postoperative complications i.e < 15% of patients have postoperative complications which include uterine perforation,fluid overload, haemorrhage & UTI, compared to 45% in hysterectomy which include haemorrhage, trauma (ureters, bladder, bowel), infection (wound, pelvic, UTI), thromboembolism & pain. Disadvantages compared to hysterectomy: 20% failure , in which the patient need another resection and ablation or hysterectomy , compared to 100% cure rate in hysterectomy. The risk of endometrial cancer still remains.
Cervical ectropion (cervical erosion) Cervical polyp. Cervical malignancy. Acute & chronic cervicitis
It is not an ulcer. It is due to the eversion of the columnar epithelium of the endocervix on the ectocervix. Occurs in the childbearing age, and most frequently during pregnancy & in COC users ,due to high oestrogen levels. Diagnosis: Symptoms: PCB ( from the traumatized fine blood vessels of the columnar epithelium) & excessive mucus non-purulent vaginal discharge ( from the mucus secreting glands of the columnar epithelium of the cervix). Speculum examination shows red granular area around the external os. Cervical smear is mandatory before treatment to exclude cervical carcinoma.
Treatment: Conservative during pregnancy & in COC users. Wait for 2-3 months after delivery & after stopping of COC. If symptoms persist after that time, treatment is by local destruction. Local destruction: The best by cryotherapy or thermal cautery.
It is a smooth pedunculated growth from the columnar epithelium of the endocervix Polyps can be due to hypertrophy of the mucus membrane or may be benign neoplasms which are of low malignant potential The surface epithelium of the polyp is often ulcerated, causing IMB or PCB with which patients most commonly present They can be avulsed by twisting, and if necessary, the base can be cauterized. The specimen should be sent for histological examination.
Aetiology: Pathological : Cervical: Erosion, polyp and carcinoma. Endometrial: Polyp and carcinoma. Vaginal: Polyp and carcinoma. Urethral: Caruncle. Contraception: Breakthrough bleeding in COC & minipill users & the irregular bleeding in IUCD. Physiological: Midcycle bleeding at the time of ovulation.
Diagnosis: History: Analysis of complaint. Duration of complaint, amount of bleeding, irregularity of bleeding and relation to menses and intercourse. Associated symptoms : PCB, menorrhagia, vaginal discharge & pain. Contraception: IUCD and hormonal contraception. Examination: Speculum examination of the cervix & the vagina. Bimanual examination of the uterine size &shape, and the adnexal masses. Investigations: U/S. Cervical smear. Hysteroscopy and D&C: if no cervical &vaginal cause can be identified. Treatment: Is according to the underlying cause.
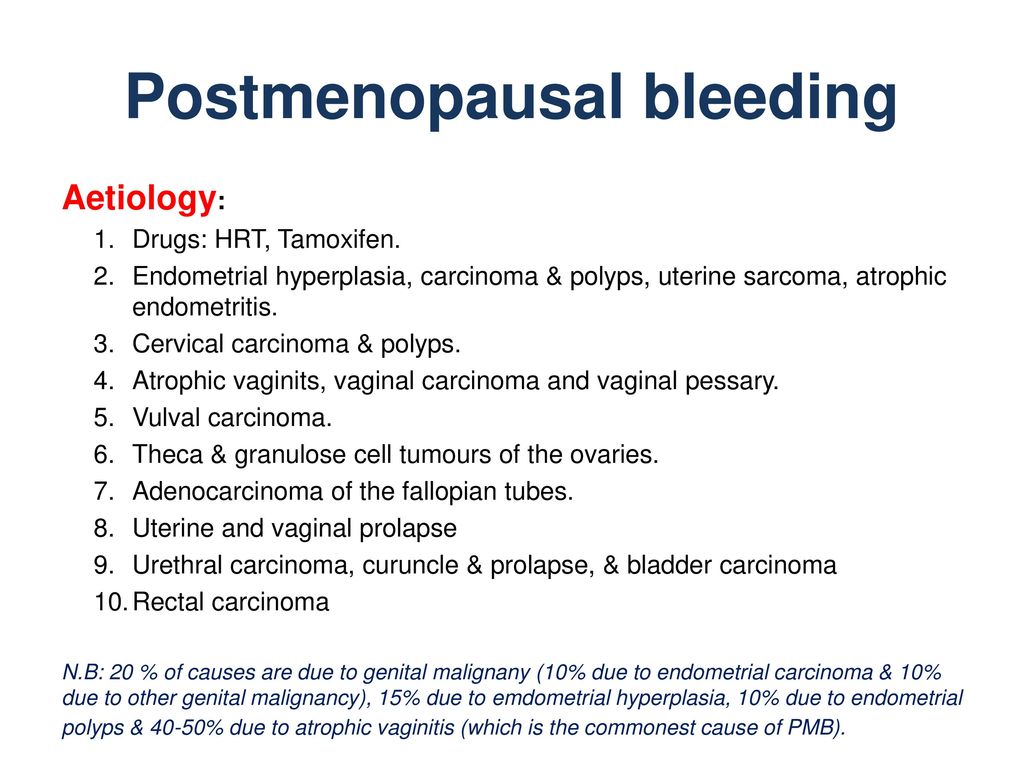
Aetiology: Drugs: HRT, Tamoxifen. Endometrial hyperplasia, carcinoma & polyps, uterine sarcoma, atrophic endometritis. Cervical carcinoma & polyps. Atrophic vaginits, vaginal carcinoma and vaginal pessary. Vulval carcinoma. Theca & granulose cell tumours of the ovaries. Adenocarcinoma of the fallopian tubes. Uterine and vaginal prolapse. Urethral carcinoma, curuncle & prolapse, & bladder carcinoma. Rectal carcinoma N.B: 20 % of causes are due to genital malignany (10% due to endometrial carcinoma & 10% due to other genital malignancy), 15% due to emdometrial hyperplasia, 10% due to endometrial polyps & 40-50% due to atrophic vaginitis (which is the commonest cause of PMB).
Diagnosis: History : A- Analysis of the complaint & associated symptoms. Duration of complaint. Amount of bleeding. Previous similar attacks. Relation to sexual activity. Associated menopausal symptoms i.e. Hot flushes and dryness of vagina. Associated : Pelvic pain , vaginal discharge and loss of weight. B- Previous investigations and treatment for her complaint. C- Gynecological history : Age of menopause. Last cervical smear. Previous gynecological operations D- Medical history : Use of HRT. History of cancer breast and use of tamoxifen.
Examination: General : General condition of the patient. Signs of malignancy such as cachexia, lymphadenopathy, abdominal masses, ascitis & lower limb oedema. Pelvic. Inspection of the vulva & urethra. Speculum examination of the cervix and the vagina, for the local causes & for signs of atrophic vaginitis ( which include dryness of vagina ,pallor, thin appearance of the mucosa & loss of the mucosal rugae). Bimanual examination of the uterine size & for adnexal masses. Investigation: U/S: the main objective is to assess endometrial thickness, and if > 4 mm is suspicious and maybe due to hyperplasia or malignancy . Fibroids and adnexal masses. Cervical Smear. Hysteroscopy & endometrial biopsy, which is mandatory if endometrial thickness is >4mm.
Treatment: If a cause is detected, treatment is that for the underlying cause. e.g.: If the bleeding is due to endometrial hyperplasia , the treatment is by TAH + BSO. If the bleeding is due to endometrial carcinoma , the treatment is by TAH + BSO, followed by postoperative radiotherapy, chemotherapy and hormonal treatment. If no cause is detected, the patient treated with HRT ( by local estrogen or combined systemic HRT ) to treat the most likely cause i.e atrophic vaginitis. If the bleeding recurs, the patient is treated by TAH& BSO, because the underlying cause may be endometrial carcinoma which is missed by D&C or rarely may be due to functioning ovarian tumours ( Theca & granulosa cell tumours), uterine sarcoma or adenocarcinoma of the fallopian tubes.
Approach to Abnormal Uterine Bleeding in General Practice - ppt video online download

ABNORMAL UTERINE BLEEDING - ppt video online download
PPT - AUB PowerPoint Presentation, free download - ID:9543767
Abnormal Uterine Bleeding
ABNORMAL UTERINE BLEEDING - ppt video online download

Approach to abnormal uterine bleeding in reproductive-aged patients: Clinical sciences - Osmosis Video Library
PPT - ABNORMAL UTERINE BLEEDING PowerPoint Presentation, free download - ID:1453413

Lymphangioleiomyomatosis: a metastatic lung disease
Abnormal uterine bleeding
What are the symptoms of cervical cancer? Abnormal vaginal bleeding is the most common symptom, but it's also important to be aware of the others. If
Queenslyn Medical Centre

Abnormal Uterine Bleeding Case Report Presentation

Miscarriage: Signs, Symptoms, Treatment And Prevention

